Questions about cancer, inflammation, and immunity : Last week, Cell Press hosted a webinar on cancer, inflammation, and immunity, which is now on demand. In it, expert scientists Douglas Fearon and Mikala Egeblad, both from the Cold Spring Harbor Laboratory, presented some of their recent research. Specifically, they discussed the complex interplay between cancer cells, immune cells and host physiology, highlighting the importance of reciprocal interactions between a tumor and a host—connections that should not be overlooked.
The discussion was insightful and we received numerous questions from listeners during the webinar, but due to time constraints, were unable to address them all. Thus, we thought this forum might provide a great opportunity to answer some of the remaining queries that were posed at the time. For the benefit of the audience, also keeping in mind individuals who expressed interest in the webinar but perhaps missed it, here are Doug and Mikala’s responses, interview style.
The Immunological Consequences of Cancer-Induced CachexiaDouglas Fearon (image courtesy of Cold Spring Harbor)
Cachexia is the fatal tumor-induced wasting syndrome characterized by progressive weight loss. In his presentation, Douglas Fearon spoke about his work in preclinical mouse models of colorectal and pancreatic cancer, exploring the link between the host’s immune and metabolic responses to cancer.
Tumor-bearing mice are impaired in their metabolic responses to caloric deficiency and a model has been proposed suggesting that a tumor can reprogram host metabolism. For example, Fearon discussed how tumor-induced IL-6 can downregulate hepatic ketogenesis (with low levels of PPARα). During caloric deficiency, hypoketonemia can then trigger glucocorticoid secretion. Elevated glucocorticoids, generated from metabolic stress, are subsequently able to suppress intratumoral CD3+ T cell immunity. This is significant because suppression of antitumor immunity can contribute to failed immunotherapy in cancer-cachectic patients.
Question 1: What do you envision are the mechanism(s) that might underlie the spontaneous loss of appetite in cancer-associated anorexia and cachexia?
Douglas Fearon: This is a key question, because without decreased caloric intake, a re-programming of PPARα (ppara) expression in the liver would have no deleterious effects. In our experiments, leptin levels were appropriately very low. We assayed the hypothalamic transcription of genes encoding known regulators of appetite, such as neuropeptide Y and AgRP (orexigenic) as well as POMC (anorexigenic), and the levels of these regulators were associated with increased food intake—that is, they were appropriate. Thus, there may be another, dominant pathway of appetite control in cachectic individuals. This may be a good project!
Question 2: How might glucocorticoids act to suppress the anti-tumor immune reaction?
DF: Glucocorticoids have many effects, so immune suppression may be multifactorial. However, we believe that one of the key events is the attraction of T cells to the tumor microenvironment, which would be mediated by chemokines. The literature suggests that CXCR3-mediated chemotaxis is important for T cell accumulation in tumors. Therefore, we’re particularly interested in the marked transcriptional downregulation—with elevated corticosterone levels—of genes encoding CXCL9, CXCL10, and CXCL11, because these are the chemokine ligands for CXCR3. I can refer you to a recent review of my thoughts about what regulates the intratumoral accumulation of T cells.
Question 3: What about lipid metabolism in your model? Does it also change, and is it involved in immunosuppression?
DF: We only studied lipid metabolism with respect to the PPARα-dependent, mitochondrial β-oxidation of free fatty acids to ketones.
Question 4: Are there any observational data on the cortisol levels of patients receiving programmed death-1 PD-1/PD-L1 checkpoint blockade?
DF: Not yet. We have indeed wondered whether maintaining the glucocorticoid levels at the physiological nadir might enhance the effects of cancer immunotherapy in mice.
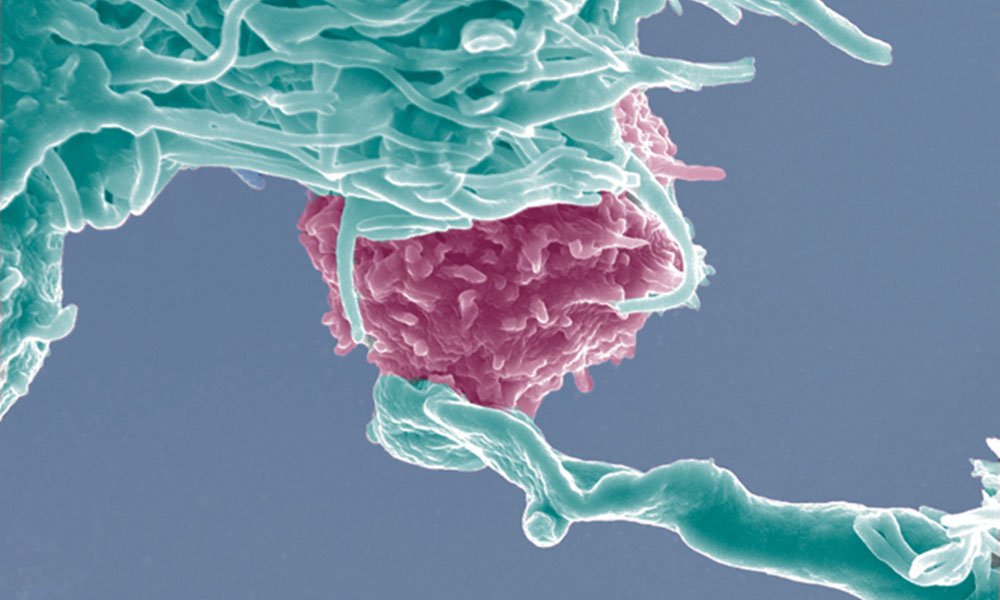
The Effects of Neutrophil Extracellular Traps on MetastasisMikala Egeblad (image courtesy of Cold Spring Harbor)
Mikala Egeblad presented recent findings on the influence of the inflammatory host environment in promoting mammary tumor metastasis. She focused on the mechanism of neutrophil killing that involves neutrophil extracellular traps (NETs): in murine models of breast cancer, neutrophils can infiltrate metastases and extracellular DNA “clouds” can surround tumor cells. Neutrophils and NET formation—empowered by tumor-cell-secreted G-CSF—can then enable cancer cell tissue invasion and increased metastasis (removing NETs via DNAse I, abrogates seeding, and metastasis). As such, the clinical and functional implications of the pro-metastatic properties of NETs are raising significant interest.
Question 1: Is there any evidence for a tumoricidal function of neutrophils?
Mikala Egeblad: Yes, there’s clear evidence that neutrophils can also be tumoricidal. Even NETs may be cytotoxic under certain conditions. However, we don’t yet understand what determines whether a neutrophil has pro- or anti-tumor functions.
Question 2: Ly-6G is also a marker for granulocytic myeloid-derived stem cells (MDSCs). Is there a difference in NET formation between mature neutrophils and MDSCs?
ME: Yes, that is correct. There are reports showing that granulocytic MDSCs can also form NETs. We have isolated Ly-6G+ cells from both naïve and tumor-bearing mice and compared the ability of these cells to form NETs. We have observed that both populations readily form NETs, but following co-culture with 4T1 breast cancer cells, there are slightly fewer NETs formed from Ly-6G+ cells that were derived from tumor-bearing mice when compared to those from naïve mice. Also, we don’t really know if there are any qualitative differences between NETs formed from mature versus immature neutrophils.
Question 3: Did you try the same experiments in mice under chronic anti-inflammatory treatment? Is there a role for low-dose aspirin in NETs? What about metformin, which has an anti-inflammatory effect, countering IL-1 and TNF?
ME: This is a great question. Others have indeed shown that aspirin can reduce platelet-induced NET formation. We have not yet performed experiments testing the effects of anti-inflammatory treatments on NET-induced metastasis.
Question 4: Carbonic anhydrase IX has been shown to induce G-CSF production. Did you try to see if hypoxia affects NET formation?
ME: We have not tested this directly, but have noticed that there are typically more NETs in tumor regions that border areas where severe necrosis is present. These regions would indeed be expected to be hypoxic.
Question 5: Could you test in your cancer models if there are changes in how NETs respond (and the mechanisms of neutrophil recruitment) in the presence or absence of a co-infection?
ME: This is a great idea, and we would like to do experiments were we would remove the primary tumor and then infect the surgical wound in order to mimic the clinical risk of wound infection after surgery. Lorenzo Ferri’s group has a nice model for co-infection and lung cancer where one could test this.
I think it’s very important to start addressing what determines whether a neutrophil becomes tumoricidal, degranulates, or forms NETs. There are some signals that have been identified and shown to affect the fate of neutrophils, but I think we still have a lot to learn about the plasticity of these cells.