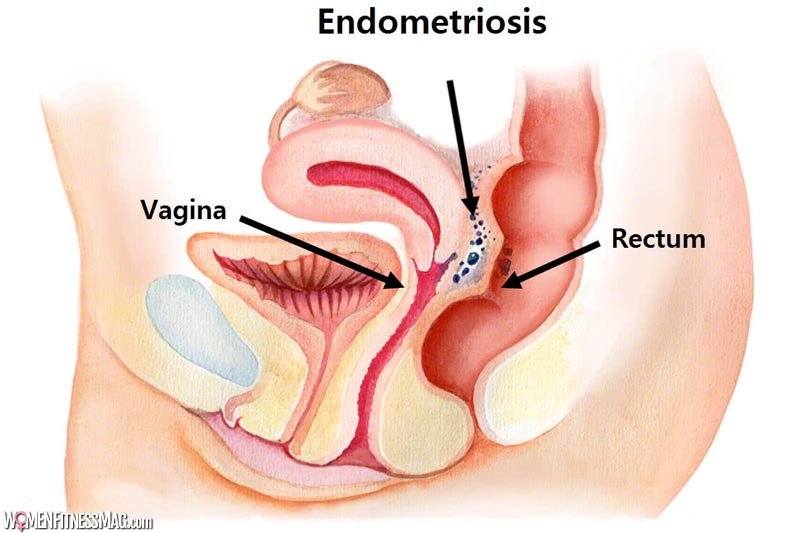
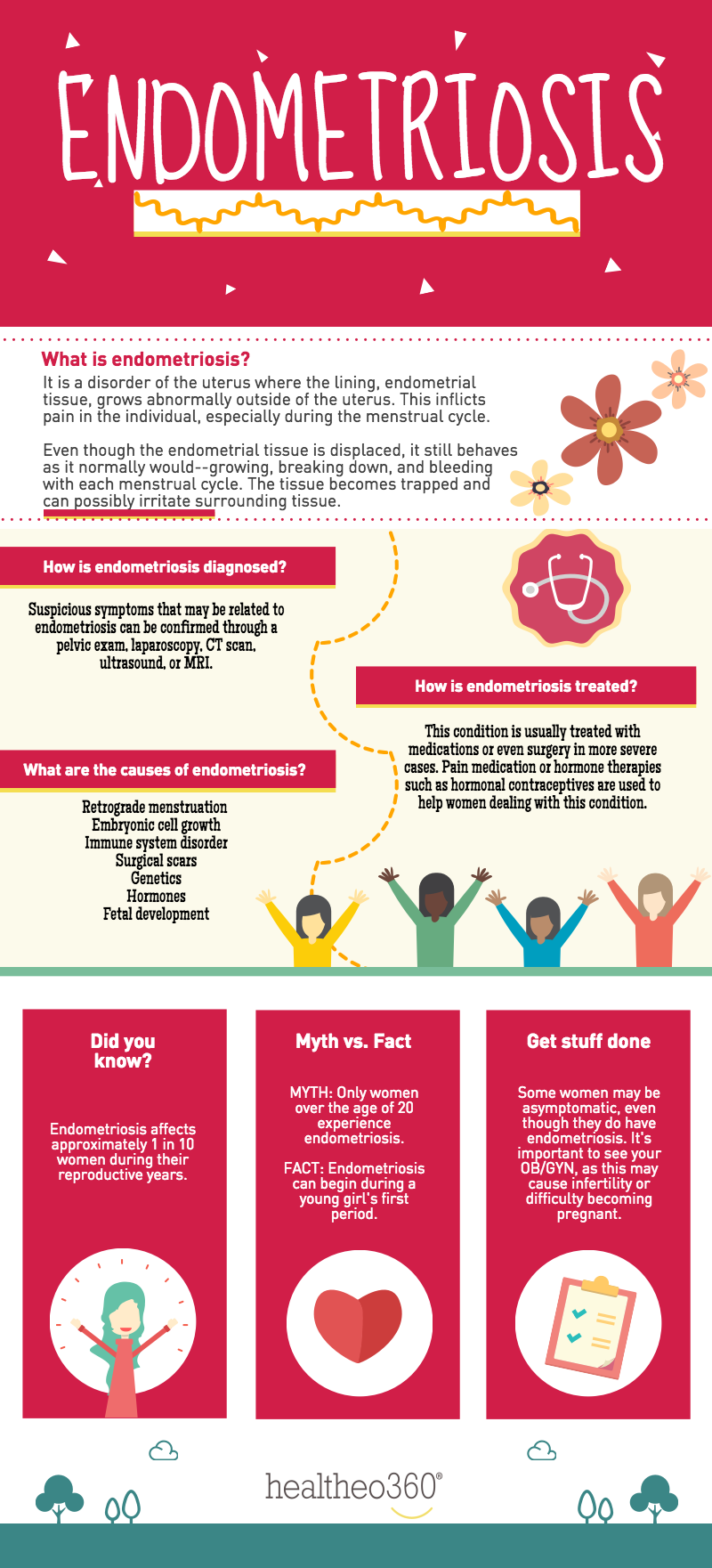
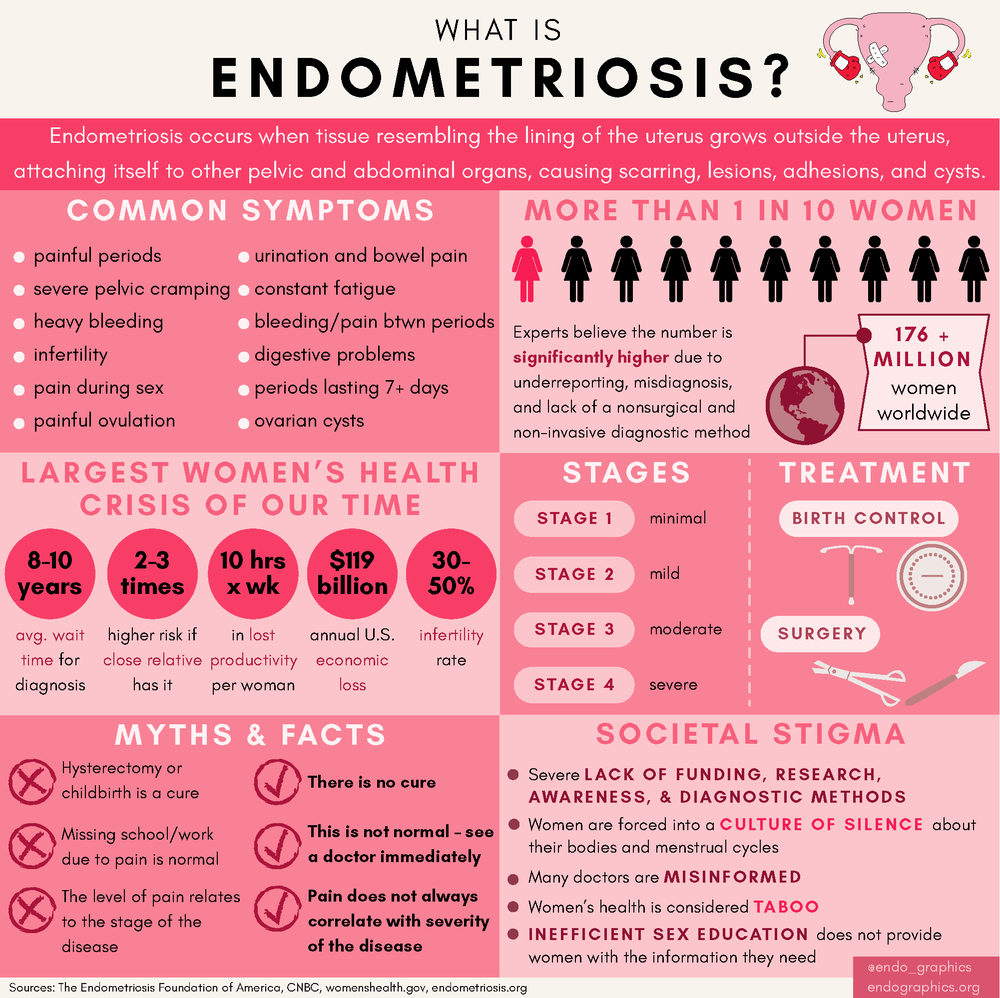
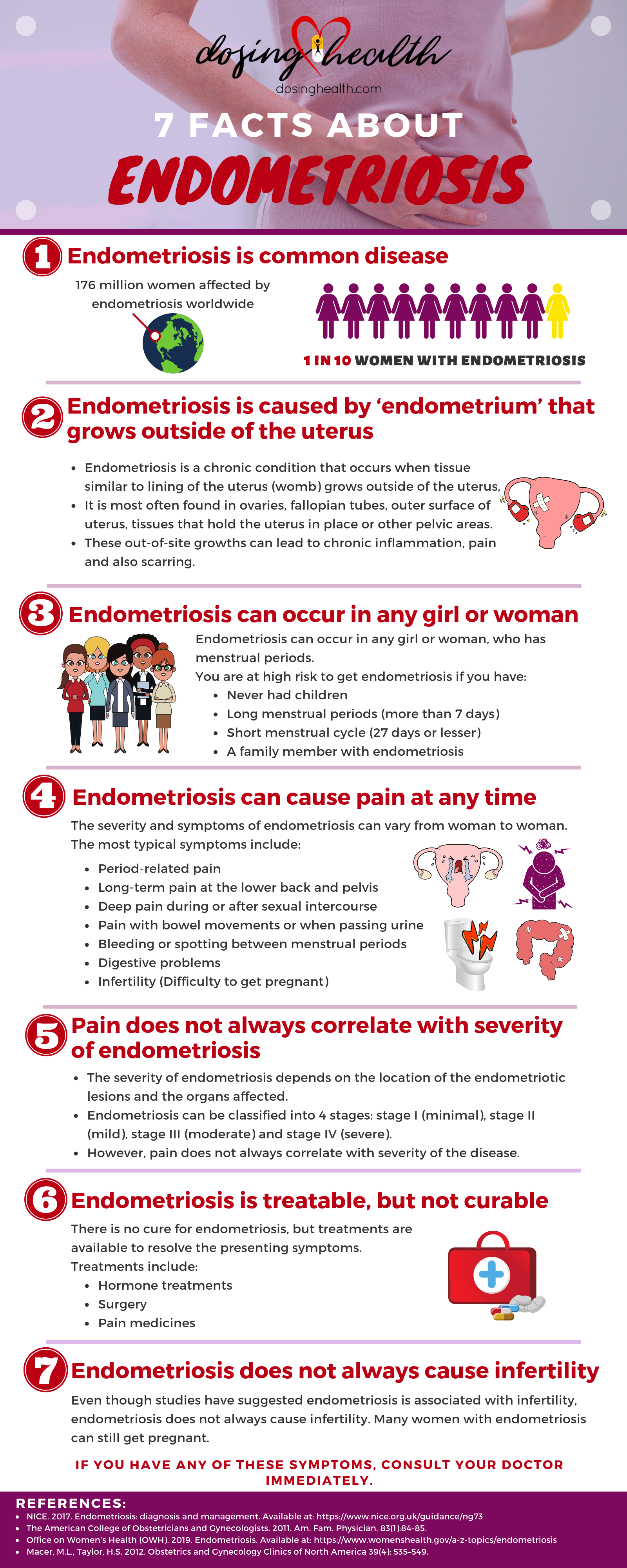
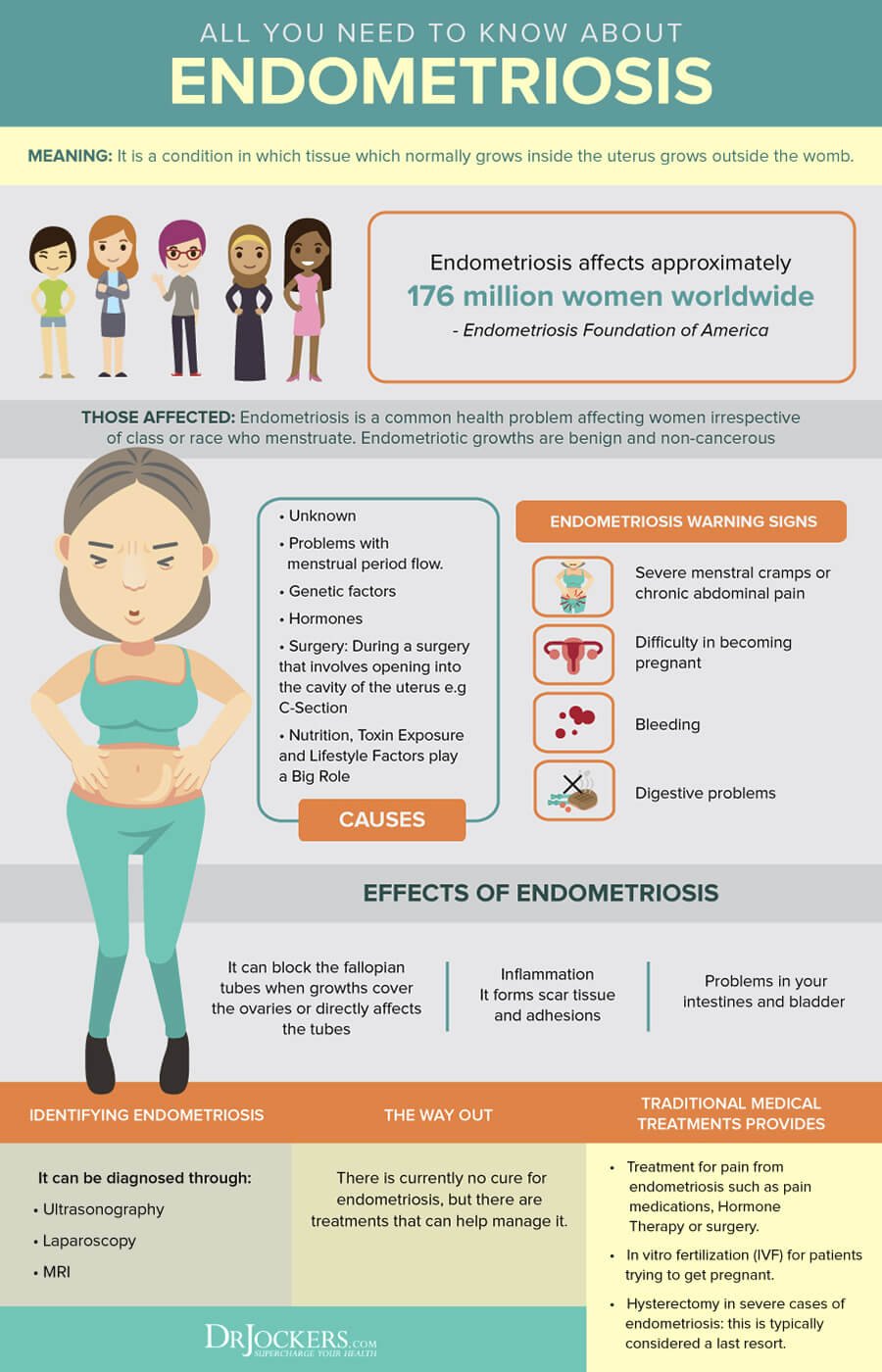
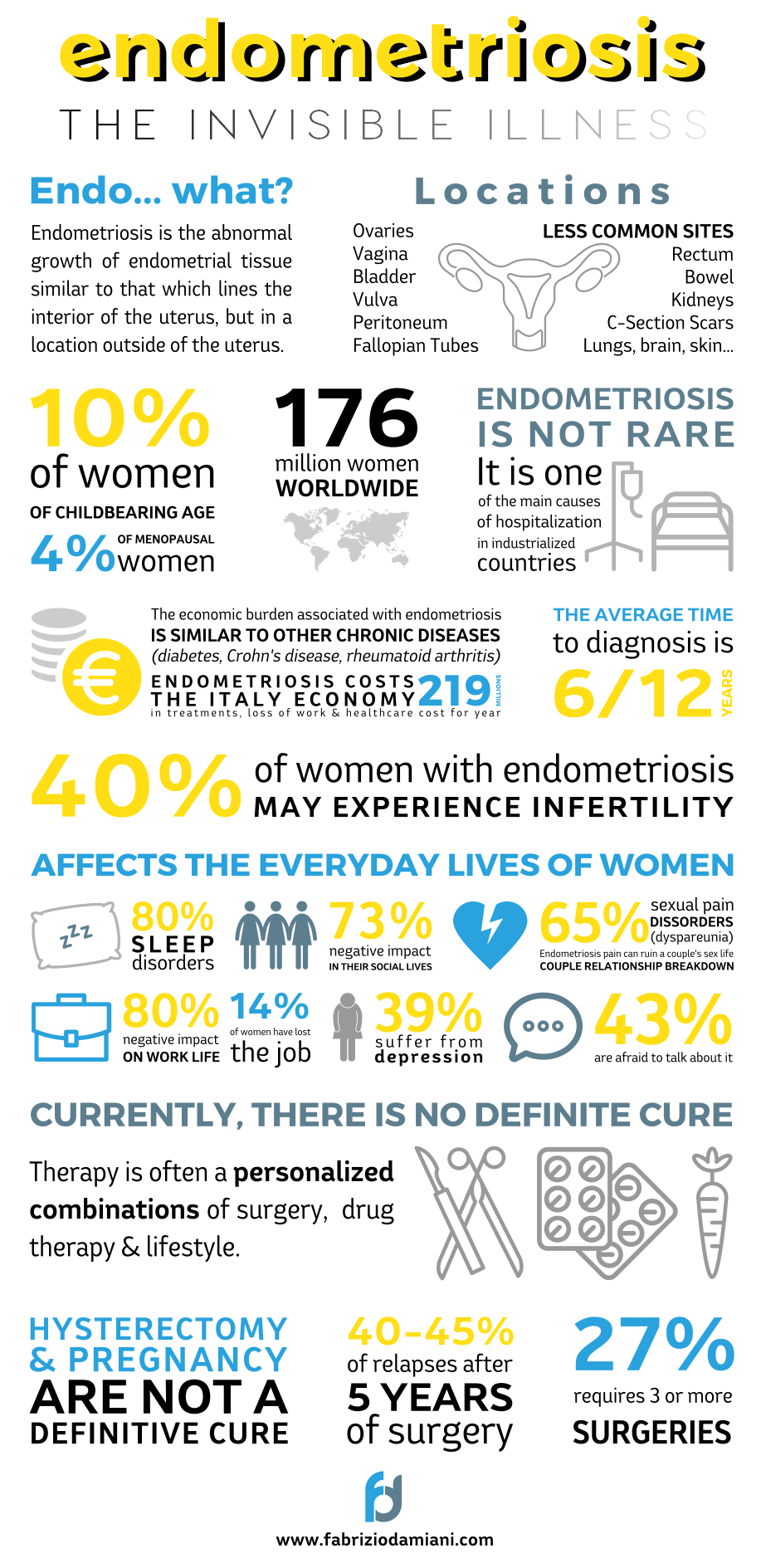
One of the most common health issues for women today is endometriosis. A very painful disorder, in which tissue similar to the endometrium tissue (which is present in the inner linings of the uterus) grows outside of the uterus. Usually, endometriosis spread over ovaries, fallopian tubes, and the tissue lining your pelvis.
Rarely, it spread beyond these areas, even in pelvic organs. Fertility specialists in India are trying their best to spread awareness regarding this.
In simple words, endometrial tissue is the one that breaks down and bleeds out along with the egg, during menstrual. So when this tissue starts forming outside of the Uterus, it thickens, breaks down, and bleeds with each menstrual cycle, but now this tissue doesn’t have any way to get out of the body, it gets trapped inside. When this disorder involves the ovaries, it results in cysts, called endometriomas. Due to this, the surrounding tissue becomes irritated. Eventually, the surrounding tissue may result in scar tissue and adhesions, or the abnormal bands of fibrous tissue (they can cause pelvic tissues and organs to stick to each other). Apart from this, endometriosis can cause severe pain, especially during menstrual periods. Even infertility is one of the complications.
According to the Endometriosis Society of India, presently, more than twenty-five million women are facing this disorder in the country. Endometriosis treatment shares a good share of female infertility treatment in India. Then Also only a handful of people are aware of this problem, the main reason for this is that it’s a taboo and an issue of embarrassment for the young ladies, so they don’t open up about it. This also leads to delay in treatments and a lack of moral and mental support to them.
In this article we will be covering:
- Symptoms
- Causes
- Risk factors
- Diagnosis
- Treatment
- What to expect from your doctor
Symptoms
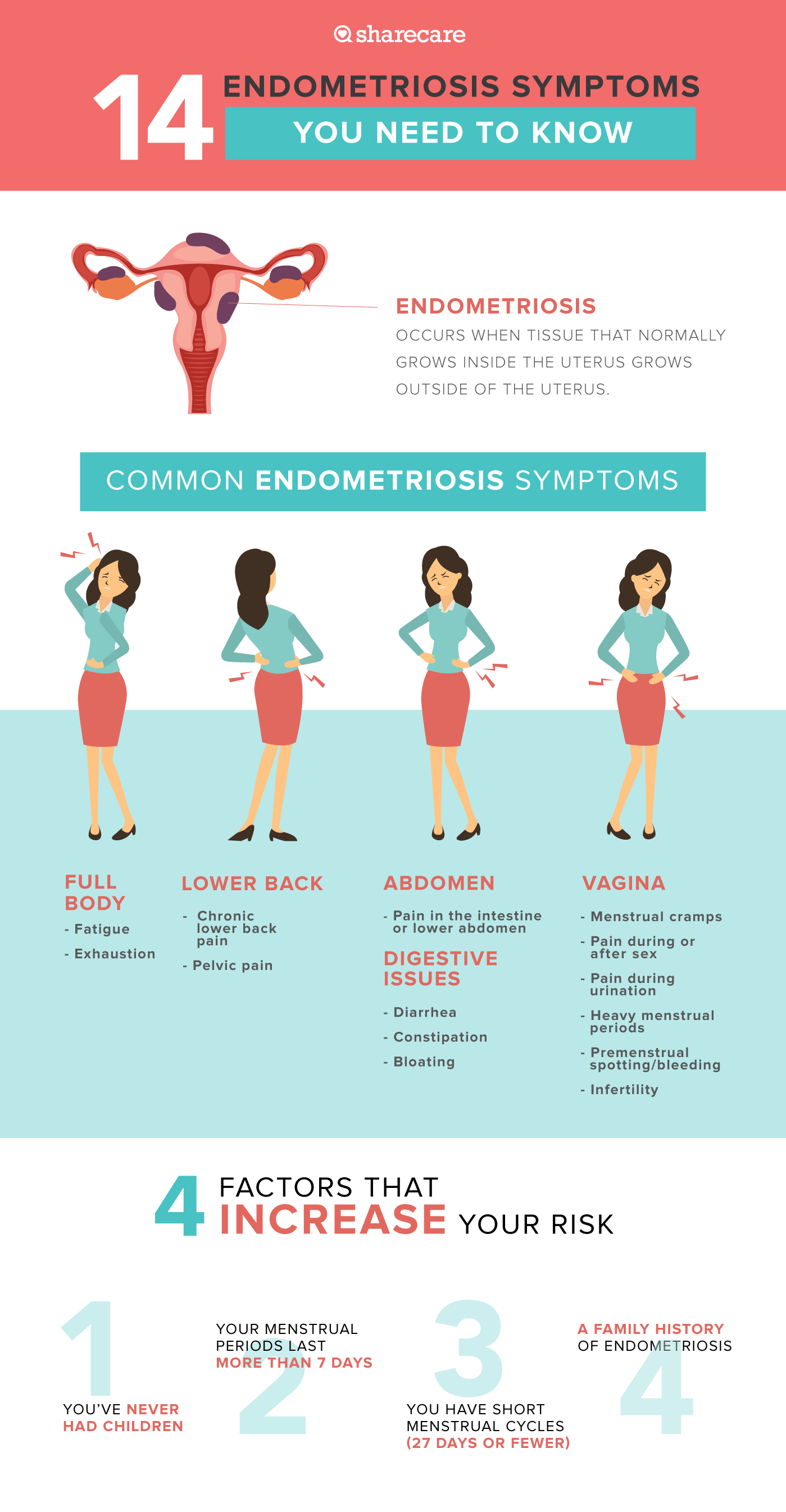
Endometriosis, as we have read, is similar to menstrual, so it’s signs and symptoms include the same for menstrual, but at a much higher intensity.
Common signs and symptoms of endometriosis include:
- Pelvic pain- It is one of the early symptoms of endometriosis. It’s often ignored as it can be associated with menstrual. The difference between a cramp and pain caused by menstrual is the intensity of the pain. Pain with endometriosis is typically far worse than usual, and can also increase with time.
- Painful periods (dysmenorrhea)- The pelvic pain may begin before and even extend after menstrual. Other than this pelvic pain, one can also experience lower back and abdominal pain.
- Pain with intercourse- Pain during or after coitus is a common sign for endometriosis.
- Pain with bowel movements or urination- As we have mentioned pelvic, abdominal and back pain above so they can cause pains during urination or bowel movement. Apart from that, this can also lead to various infections.
- Excessive bleeding- As explained, the tissue thickens and breaks outside the Uterus, so instead of getting trapped it might flow out with the blood too. Women anyways shouldn’t ignore heavy menstrual or intermenstrual.
- Infertility- It is one of the severe and common symptoms of endometriosis. For many ladies, their endometriosis gets detected during their infertility diagnosis only. As the disorder affects ovaries, fallopian tubes, and uterus so it is bound to affect fertility too.
- Other signs and symptoms- Experiencing fatigue, diarrhea, constipation, bloating, or nausea, are other signs and symptoms.
Remember, the severity of the pain isn’t surely an indicator of the extent of the condition. Some women experience severe pain during mild endometriosis, while some experience only little of it even with the advanced endometriosis.
Often, endometriosis is mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It may be confused with irritable bowel syndrome (IBS) too, as the condition causes bouts of diarrhea, constipation, and abdominal cramping. If IBS accompanies endometriosis, this can complicate the diagnosis.
Causes
The cause of endometriosis is not certain. There are various supported theories for the same. Doctors use them as the contour for initiating the treatment. Listed below are the possible explanations include:
- Retrograde menstruation- In this menstrual blood (which contains endometrial cells) flows back through the fallopian tubes into the pelvic cavity, instead of out of the body. Then, these endometrial cells stick to the pelvic walls and the surfaces of pelvic organs. They then grow, continue to thicken, and then bleed with each menstrual cycle.
- Transformation of peritoneal cells- Experts propose that endometriosis can also be caused by hormones or immune factors promoting the transformation of peritoneal cells (cells that line the inner side of the abdomen) into endometrial-like cells.
- Embryonic cell transformation- Estrogen, a hormone, with others, may transform embryonic cells (cells in the earliest stages of development) into endometrial-like cell implants. The resulting implants have all the characteristics like ones that grow during puberty.
- Surgical scar implantation- After surgeries (like in, hysterectomy or C-section) endometrial cells can attach to a surgical incision and grow accordingly.
- Endometrial cell transport- Sometimes the blood vessels or the tissue fluid (lymphatic) system, may transport endometrial cells to other parts of the body.
- Immune system disorder- In this, the immune system of the lady might be hampered. This makes the body unable to recognize and destroy endometrial-like tissue which is growing outside the uterus.
Risk factors
Apart from the above causes, mentioned below are a few factors that have proved to be a catalyst in developing endometriosis:
- Choosing to never give birth
- Commencement of periods at an early age
- Commencement of menopause at an older age
- Short menstrual cycles (less than 27 days
- Heavy menstrual periods that also last for more than seven days
- Having high levels of estrogen (also if the release of estrogen is a lot more than usual)
- Lower body mass index
- Blood relatives having endometriosis
- Any medical condition that prevents the normal menstrual flow out of the body
- Abnormalities in the reproductive tract
Diagnosis
When you will consult the doctor about your issue. To diagnose whether it’s endometriosis or the other condition, they will ask you to describe your signs and symptoms. Describe all the symptoms or causes you believe you are going through. An accurate and sharp description will help in diagnosis more than you can even imagine.
Tests for diagnosing endometriosis include:
- Pelvic exam- The doctor palpates the areas in your pelvis for checking any abnormalities, such as cysts on the reproductive organs or the scars behind the uterus. Unless a cyst(s) is formed it’s not possible to feel small areas.
- Ultrasound- It is a high-frequency sound wave test, they help in creating images of the inside of the body. For capturing images, a device called a transducer is either pressed against the abdomen or inserted into the body (transvaginal ultrasound). A standard ultrasound imaging test is for identifying cysts associated with endometriosis (endometriomas). These tests don’t precisely tell whether the patient has endometriosis or not.
- Magnetic resonance imaging (MRI)- Through it, the detailed images of the organs and tissues within your body are created. This is done with the magnetic field and radio waves. For some, an MRI helps with surgical planning, giving a surgeon detailed information about the location and the size of endometrial implants.
- Laparoscopy- In some cases, the doctor refers to a surgeon for this. It is a procedure to view the inside of the abdomen (laparoscopy). The patient is given general anesthesia, the surgeon makes a tiny incision near the navel to insert a slender viewing instrument (laparoscope), they look for the signs of endometrial tissue outside the uterus. Laparoscopy can provide information about the location, extent, and size of the endometrial implants. The surgeon may take a tissue sample (biopsy) for further testing. Often, with precise surgical planning, the surgeon can fully treat endometriosis.
Treatment
The treatment for endometriosis involves both medication and surgery. The doctor/surgeon will use the specific approach and technique after diagnosing the severity of the condition and whether the patient wants to be pregnant or not. Often a doctor will recommend conservative treatment approaches first and will opt for surgery if the initial treatment fails.
Pain medication
Your doctor may recommend that you take an over-the-counter pain reliever, or may prescribe you the same. It is always beneficial to get a prescribed painkiller. They are for reducing the cramp pains, pelvic pain, abdominal pain, and back pain. They may/may not be used in hormonal therapy.
- Hormone therapy- In some cases, hormone supplements are used to reduce or eliminate the pain. As the rise and fall of hormones during the cycle causes endometrial implants to thicken, break down, and bleed, therefore the hormone medication may slow endometrial tissue growth and prevent new implants of endometrial tissue. Hormone therapy isn’t a permanent solution though. These therapies are:
- Hormonal contraceptives- Contraception pills, patches, and vaginal rings help to regulate the hormones liable for the buildup of endometrial tissue. Many women experience lighter and shorter menstrual flow when they use a hormonal contraceptive. Using hormonal contraceptives may decrease or eliminate pain in some cases.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists- These drugs prevent the production of ovarian-stimulating hormones, reducing estrogen levels and checking menstruation. This shrinks the endometrial tissue. As these drugs create an artificial menopause, often, a low dose of estrogen or progestin is suggested to decrease menopausal side effects, such as hot flashes, vaginal dryness, and bone loss. The periods and the ability to conceive returns when you stop taking the medication.
- Progestin therapy- There are a variety of progestin therapies to stop menstrual periods and the growth of endometrial implants. These may also include endometriosis signs and symptoms. These therapies may include an intrauterine device with levonorgestrel (Mirena, Skyla), contraceptive injection (Depo-Provera), the contraceptive implant (Nexplanon), or progestin pill (Camila).
- Aromatase inhibitors- They are a class of medicines that reduce the amount of estrogen in the body. The doctor may recommend an aromatase inhibitor and a progestin, or a combination of hormonal contraceptives to treat endometriosis.
- Conservative surgery- This surgery is for those females who are looking forward to being pregnant post-surgery. Post surgery there are high chances of pain to return. This procedure can also be performed laparoscopically or, less commonly, through traditional abdominal surgery in more extensive cases. Today, critical cases of endometriosis can also be treated with laparoscopic surgery. (In laparoscopic surgery, the surgeon inserts a slender viewing instrument (laparoscope) through a small incision near the navel and inserts instruments to remove endometrial tissue through another small incision. After surgery, the doctor generally continues with hormone medication to improve pain.
- Fertility treatment- This treatment isn’t a cure of endometriosis but infertility it causes. As discussed above, this disorder leads to trouble in conceiving. In this, the doctor recommends IVF treatment, hormone stimulation in ovaries (for producing more eggs), IUI, and more. IVF treatment in India is highly regarded because of its affordability and effectiveness. In IVF treatment the doctor retrieves the egg and sperm from the couple, fertilizes them artificially (outside the human body), and then implants a healthy embryo inside the women.
- Hysterectomy with removal of the ovaries- This is a surgery to remove the uterus (hysterectomy) and ovaries (oophorectomy). At a period, it was considered the most effective method for treating endometriosis. Today, endometriosis experts are focusing on the careful and thorough removal of all endometriosis tissue rather than extracting out these essential reproductive organs. As menopause is caused by the removal of ovaries, so it isn’t the primary option for young women. An advantage of it is that the lack of hormones produced by the ovaries helps in improving endometriosis pain for some. While for some, endometriosis remains, even after the surgery. Other than this, early menopause also brings a risk of heart and blood vessel (cardiovascular) diseases, certain metabolic conditions, which may result in early death. In the case of the removal of the uterus (hysterectomy), often it results in the total treatment of endometriosis. For women who don’t want to be pregnant in the future, removing uterus but keeping ovaries is a good option. This will result in less menstrual bleeding and painless menses (as cramping is caused by uterine, which is removed).
What to expect from your doctor
OB-GYNs are the medical experts to be approached for the treatment of endometriosis. Some are physicians while some are even surgeons along with it. Below we are mentioning some questions that you should browse before consulting a doctor, or you can even ask these in the first consultation:
- How did you diagnose endometriosis?
- How will these medications affect my body? Have you checked for the effects of them on my body type?
- What are the side effects of this medication?
- Under what circumstances is surgery recommended?
- Will endometriosis affect my ability to become conceive?
- Can treatment of endometriosis affect my fertility?
- Are there any alternatives to the treatments?
Below are the questions that you should be ready to answer to the doctor:
- For how long have you been experiencing these symptoms?
- How severe is your pain?
- Does anything make your symptoms worse?
- Do you feel any pain during coitus?
- Do you feel any pain during urination or bowel movement?
Find a doctor with whom you feel comfortable, as it is crucial in the management and treatment of endometriosis. If you feel like having a second opinion, then don’t rush with the treatment. Make sure that you know all of your options and the possible outcomes.
Related Videos about What is endometriosis? How does it affect fertility?
What is endometriosis and does it affect fertility?
Causes of endometriosis
Endometriosis and Fertility: Symptoms & Treatment
How Endometriosis affects fertility
Getting pregnant when you have endometriosis.
How Endometriosis Affects Fertility
Related Infographics about What is endometriosis? How does it affect fertility?

What is endometriosis? How does it affect fertility?
endometriosis treatment, endometriosis test, endometriosis causes, pictures of endometriosis, endometriosis stages, endometriosis cyst, how to explain endometriosis pain, endometriosis nhs, endometriosis surgery, endometriosis blood test, endometriosis symptoms quiz, endometriosis bowel,